Patient Area
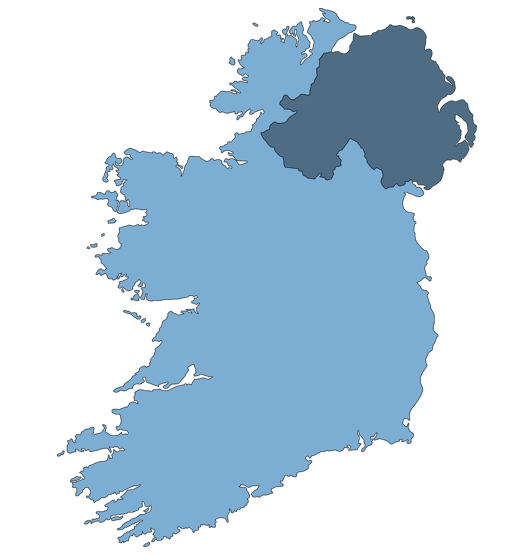
Our Network was set up to connect Inflammatory Bowel Disease researchers across Ireland. This includes consultants, nurses and research coordinators based in hospitals throughout the island of Ireland. We hope that by improving the connections and communication between research centres we will attract more clinical research studies from large sponsors in Europe and further afield. This will mean that our IBD patients will have access to new and exciting treatments, as well as establishing Ireland as an international centre for IBD research.
As an IBD patient you may have discussed participation in research studies or clinical trials with your GP or IBD consultant previously. Research studies and trials will have strict inclusion and exclusion criteria; therefore your age, symptoms, medical history, medications or some other factor may mean that you are eligible or not eligible for a certain study. If you are interested in participating in one of our studies, please feel free to discuss it with your physician to assess your eligibility, or contact us directly at initiativeibd@gmail.com.
Frequently Asked Questions 
Q: What kind of research studies do you conduct?
Our network will mostly participate in Phase 2, 3, and 4 clinical trials, observational studies, and retrospective studies. The research teams that you will meet during these studies will usually consist of consultant gastroenterologists, research nurses, IBD nurses and research coordinators.
Clinical trials involve testing a new drug to examine how effective it is at treating the target disease, and also to identify any side effects. A drug will go through four phases of trials;
Phase I:
Phase 1 trials will test the safety of a new drug, looking at any side effects that occur at different doses. These trials usually involve a small number of healthy volunteers (around 20-100) and will last several months.
Phase II:
Phase 2 trials test new drugs that have passed phase 1 trials in larger groups of people (around 100-300) who have an illness, e.g. IBD, to see if it shows signs of being an effective treatment. In this phase researchers will also examine possible side effects and try to establish the right dose of the drug to administer to patients. Phase 2 trials usually last up to 2 years.
Phase III:
If Phase 1 and 2 trials suggest the new drug may be effective, the drug will enter Phase 3 trials. Phase 3 trials compare new drugs with either a medication that is currently in use or with no drug treatment at all. They can last a year or more longer than phase 2 trials. Usually large numbers of patients (1000-3000) in different countries will participate in a phase 3 trial.
Phase IV:
Phase 4 studies are carried out after a drug has been approved and are designed to evaluate the long term effects of the drug as well as to continue looking for any previously unidentified side-effects. These trials will usually involve several thousand participants and will last for one or more years.
As well as clinical trials, where the participant will receive a dose of a drug that is different to their normal treatment, we will also be conducting observational and retrospective studies where no additional treatment is be given.
Observational Studies:
In an observational study researchers will observe patients who are already receiving a certain drug or treatment and compare them to a group who are receiving a different treatment or no treatment at all. This may be to look at the effect of a drug on a disease over time or to analyse the safety of a drug with continued use. Depending on the study protocol the patient may have to fill in a diary or questionnaires over a certain period of time tracking their disease, medications, and general well-being.
Retrospective Studies:
In a retrospective study researchers will look at the drugs or treatments that a group of people have received in the past. They will examine how the patient was while they were taking the treatment to determine if it poses any risk or if it has a protective effect. This may involve looking at medical records or asking the patient questions. This type of study will involve the least patient participation as information is mostly gathered through documents and records from the past.
Q: Do I have to pay for the drug in a clinical trial?
If you volunteer for a clinical trial where a treatment is given that is not your usual IBD treatment, the cost will be covered by the study sponsor (usually the pharmaceutical company that makes the drug). You will not have to pay anything towards the treatment.
Q: Are research studies and clinical trials regulated?
The study sponsor will put together a protocol describing every detail of the study. This will be submitted to the Health Products Regulatory Authority (HPRA) and reviewed by an Ethics Committee. The role of an ethics committee is to ensure that research is carried out so that the dignity, rights, safety and well-being of the people who take part are completely respected and protected. The HPRA and the Ethics Committee may suggest changes to a protocol before giving it their final approval.
Q: What happens during a study?
Every study will have a different protocol and therefore what is required of you will vary depending on which study you volunteer for.
Initially there will be a “screening visit” where the consultant or research nurse will assess whether you are eligible to take part in the study. You will be given an informed consent form to read. This will explain the purpose of the study, who is involved, all procedures that will occur and any possible risks and/or benefits to you when participating in the study. Signing this indicates that you have been fully informed about the study and have had sufficient time to think about whether you want to participate. Signing an informed consent form is not a promise that you will participate. You can still withdraw at any time if you decide you do not want to continue. You will usually get a copy of this consent form to keep for your own records.
Studies will usually require a “baseline visit” during which your physician will ask you questions such as your age, address, date of birth, what type of disease you have etc. They may also do a physical exam or collect samples, e.g. blood, urine, etc. This will establish where you started, so they can compare these to the same measurements at the end of the study.
During the study you may have more tests or samples collected periodically, again depending on the individual study protocol. Sometimes the tests are carried out as part of your routine care but other studies may require extra clinic visits and procedures. Some studies may require you to make changes to your everyday life. This may include avoiding certain things, e.g foods, medications etc, or taking a new investigational treatment for your IBD.
You may also be asked to keep a diary or complete questionnaires during the course of a study. This could contain notes about your general health and wellbeing, medications taken in a certain time period, any side-effects or illnesses or other factors relevant to the study.
Q: Why should I participate?
There are many reasons you may consider participating in clinical research. You may have tried many treatment options that have been unsuccessful and wish to try a new investigational treatment, or you may feel that your disease progress and treatment may be more closely monitored if you are enrolled in a clinical study. Perhaps you simply wish to contribute to research that may lead to improved treatments and care for IBD patients in the future. You should always consider the benefits and risks when thinking about participating in a clinical research study and discuss it with your GP, IBD consultant, a family member or a friend.
Q: Can I withdraw from a study?
Yes. You can withdraw from a study at any time. Furthermore, your consultant may withdraw you from a study if they feel it is in your best interest. This will not affect your future care. Some studies may require you to complete an ‘early exit’ clinic visit and the research team may still follow up with you for your safety.
Q: What happens to my samples/information during and after a study?
During a clinical study, confidentiality is a high priority. Usually the only people who will be aware that you are participating in a study will be the doctor and research nurse/coordinator looking after you in the trial, and your GP.
During the trial and in any published results, all of your information will be kept confidential. Usually a study will assign each participant a number or code which will be used instead of their name throughout the study. The protocol for each study will clarify what will happen to your samples and information after the study closes, i.e. how long samples and information must be kept, where they are stored and how they are to be destroyed. If samples and/or information are to be used after the study has finished this must be detailed in the original study protocol and in the informed consent form you will read and sign.
Q: What if I develop a side effect?
If you are taking a drug for a clinical trial and you have a negative reaction to the drug, you should contact the consultant or research nurse/coordinator who is looking after you for the trial. He/she will assess your symptoms and may choose to withdraw you from the trial. He/she will then review your treatment plan and decide how best to proceed. The study sponsor will also be informed and may choose to suspend the trial depending on the severity of the reaction and how many participants have been affected.
Q: What if I get chosen to receive a placebo?
In some clinical trials, patients are randomly assigned to receive either the drug being tested or a placebo. A placebo will look like the drug but will contain no actual medication. This allows the investigators to compare the IBD symptoms and side effects in people receiving the real drug to people who are not receiving the drug. Usually this type of trial is blinded, meaning that neither the investigator nor the patient will know which treatment the patient was assigned. This keeps the trial fair and free of bias.
Researchers choose to use a placebo rather than giving the patient no treatment at all to test for a ‘placebo effect’. This is when people who are taking a pill or other treatment will feel better just because they think the treatment is helping them, even if it contains no active ingredient. For example if the same number of people in a placebo group and in a drug-treated group feel better after taking their treatment, this shows that the drug is not having a real effect on the disease.
Most clinical trials will offer a course of the real drug to patients from the placebo group after the trial finishes or if they have a flare of their IBD symptoms and have to exit the trial. This is known as open-label treatment, i.e. both the patient and investigator know what treatment the patient is receiving.
Q: Will I find out the results?
Depending on the type of study, it can take several years for results to be published. If you are thinking of participating, or are participating in a study and would like information on the results, ask the consultant who will be/is looking after you how long it will be until results are released and how you go about obtaining this information.
Q: How do I volunteer for a study?
If you are interested in participating in any of our studies please discuss this with your IBD consultant to establish if you are eligible and to weigh up the pros and cons. If your physician is not involved in the study that you are interested in, you can pass on details of our website and/or email address and they can then contact us to discuss your participation in the study in question.
Alternatively you can contact us directly at initiativeibd@gmail.com and we can discuss your eligibility with you and contact your physician as necessary. If you are then accepted as a participant you would see a consultant and/or research nurse in a hospital that is participating in the study for your study visits and procedures.